Introduction: Krüppel-like factor-2 (KLF2) is a critical nodal transcription factor and a tonic repressor of myeloid cell activation. Loss of KLF2 is associated with a pro-inflammatory and pro-thrombotic state. Mice deficient in myeloid-KLF2 (MK2KO) experience significantly higher mortality from lipopolysaccharide (LPS), and have increased serum and tissue levels of pro-inflammatory cytokines such as IL-1β. IL-1β is a product of NLRP3 inflammasome priming and activation, which has been implicated in numerous inflammatory and immune-mediated diseases. Neutrophils are the first responders of the innate immune system and are responsible for bacterial antigen detection. We thus aimed to elucidate the role of KLF2 in the regulation of NLRP3 inflammasome activation and subsequent IL-1β release in the neutrophil compartment.
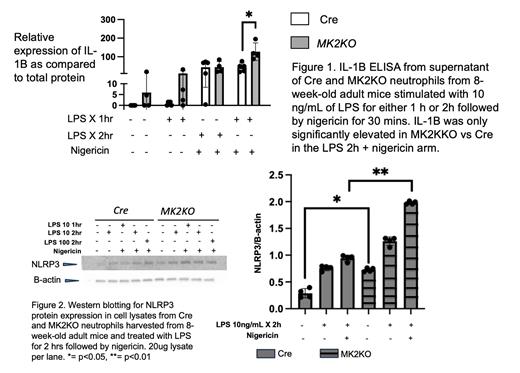
Methods: 8-week old adult MK2KO ( Lyz2Cre/ Klf2fl/fl) and control ( Lyz2Cre) mice were used for obtaining neutrophils from the bone marrow. Neutrophils were plated in RPMI-1640 media and stimulated with 10 ng/mL of LPS for 1 hour (h) and 2 h, followed by nigericin for 30 minutes. LPS acts as a priming agent for NLRP3 inflammasome assembly, and nigericin is a potassium ionophore which enables the activation step and subsequent IL-1β release. Supernatant was used for IL-1β ELISA and cell lysate was used for protein extraction and Western blotting to quantify NLRP3 protein expression. GraphPad Prism was used for statistical analyses.
Results: Neutrophils from both MK2KO and Cre mice have significantly increased production of IL-1β when stimulated with LPS followed by nigericin (Figure 1), and loss of KLF2 leads to significantly increased IL-1B release from neutrophils. MK2KO neutrophils also have significantly more NLRP3 protein expression as compared to Cre neutrophils at baseline, and in response to LPS and nigericin (Figure 2). This increase in NLRP3 protein expression was time dependent and dose-dependent (Figure 2).
Conclusion: KLF2 negatively regulates the transcriptional expression of NLRP3 and loss of KLF2 leads to increased NLRP3 inflammasome priming, at baseline and in response to LPS. Loss of KLF2 also affects the second step of the NLRP3 inflammasome pathway - the activation step, leading to increased IL-1β release in neutrophils in adult mice. Ongoing studies are examining the mechanisms underlying KLF2 control of NLRP3 transcription and other aspects of inflammasome activation. Inflammasome activation has been implicated in sepsis-related mortality due to the pro-inflammatory cytokine storm, and thus modulating KLF2 might help in developing novel targets to reduce this burden of mortality.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal